Mazumder T, Akter E, Rahman SM, Islam MT, Talukder MR. Prevalence and Risk Factors of Gestational Diabetes Mellitus in Bangladesh: Findings from Demographic Health Survey 2017-2018. Int J Environ Res Public Health. 2022;19(5).
Zhu H, Zhao Z, Xu J, Chen Y, Zhu Q, Zhou L, et al. The prevalence of gestational diabetes mellitus before and after the implementation of the universal two-child policy in China. Front Endocrinol (Lausanne). 2022;13:960877.
Zhou T, Du S, Sun D, Li X, Heianza Y, Hu G, et al. Prevalence and Trends in Gestational Diabetes Mellitus Among Women in the United States, 2006-2017: A Population-Based Study. Front Endocrinol (Lausanne). 2022;13:868094.
Pokharel P, Pokhrel KM, Lamichhane P, Khanal K, Rawal S. Prevalence of Gestational Diabetes Mellitus in Nepal: A Systematic Review and Meta-analysis. J Nepal Health Res Counc. 2022;20(1):12-20.
Meyer BN, Cash HL, Uso A, Eliapo-Unutoa I, Ropeti R, Muasau-Howard B. Gestational Diabetes Mellitus Prevalence, Screening, and Treatment Practices in American Samoa, 2016. Hawaii J Health Soc Welf. 2022;81(7):185-92.
Song S, Zhang Y, Qiao X, Duo Y, Xu J, Peng Z, et al. ALT/AST as an Independent Risk Factor of Gestational Diabetes Mellitus Compared with TG/HDL-C. Int J Gen Med. 2022;15:115-21.
Benhalima K, Van Crombrugge P, Moyson C, Verhaeghe J, Vandeginste S, Verlaenen H, et al. Risk factor screening for gestational diabetes mellitus based on the 2013 WHO criteria. Eur J Endocrinol. 2019;180(6):353-63.
Tsakiridis I, Giouleka S, Mamopoulos A, Kourtis A, Athanasiadis A, Filopoulou D, et al. Diagnosis and Management of Gestational Diabetes Mellitus: An Overview of National and International Guidelines. Obstet Gynecol Surv. 2021;76(6):367-81.
Homayouni A, Bagheri N, Mohammad-Alizadeh-Charandabi S, Kashani N, Mobaraki-Asl N, Mirghafurvand M, et al. Prevention of Gestational Diabetes Mellitus (GDM) and Probiotics: Mechanism of Action: A Review. Curr Diabetes Rev. 2020;16(6):538-45.
Szmuilowicz ED, Josefson JL, Metzger BE. Gestational Diabetes Mellitus. Endocrinol Metab Clin North Am. 2019;48(3):479-93.
Russ JB, Simmons R, Glass HC. Neonatal Encephalopathy: Beyond Hypoxic-Ischemic Encephalopathy. Neoreviews. 2021;22(3):e148-e62.
Yildiz EP, Ekici B, Tatli B. Neonatal hypoxic ischemic encephalopathy: an update on disease pathogenesis and treatment. Expert Rev Neurother. 2017;17(5):449-59.
Chiang MC, Jong YJ, Lin CH. Therapeutic hypothermia for neonates with hypoxic ischemic encephalopathy. Pediatr Neonatol. 2017;58(6):475-83.
Bonifacio SL, Hutson S. The Term Newborn: Evaluation for Hypoxic-Ischemic Encephalopathy. Clin Perinatol. 2021;48(3):681-95.
Rossi AC, Prefumo F. Antepartum and intrapartum risk factors for neonatal hypoxic-ischemic encephalopathy: a systematic review with meta-analysis. Curr Opin Obstet Gynecol. 2019;31(6):410-7.
Kureshi A, Khalak R, Gifford J, Munshi U. Maternal Obesity-Associated Neonatal Morbidities in Early Newborn Period. Front Pediatr. 2022;10:867171.
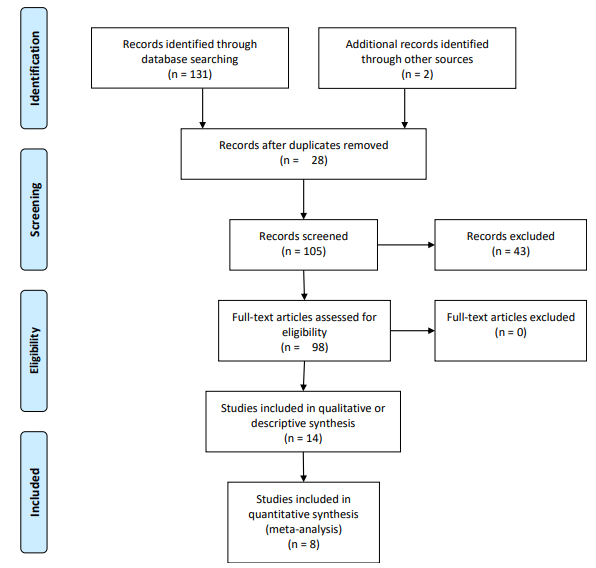
Parums DV. Editorial: Review Articles, Systematic Reviews, Meta-Analysis, and the Updated Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) 2020 Guidelines. Med Sci Monit. 2021;27:e934475.
Bano S, Chaudhary V, Garga UC. Neonatal Hypoxic-ischemic Encephalopathy: A Radiological Review. J Pediatr Neurosci. 2017;12(1):1-6.
Villamor E, Tedroff K, Peterson M, Johansson S, Neovius M, Petersson G, et al. Association Between Maternal Body Mass Index in Early Pregnancy and Incidence of Cerebral Palsy. JAMA. 2017;317(9):925-36.
Monaco-Brown M, Munshi U, Horgan MJ, Gifford JL, Khalak R. Association of Maternal Obesity and Neonatal Hypoxic-Ischemic Encephalopathy. Front Pediatr. 2022;10:850654.
AlMuqbil M, Alanazi J, Alsaif N, Baarmah D, Altwaijri W, Alrumayyan A, et al. Clinical Characteristics and Risk Factors of Neonatal Hypoxic-Ischaemic Encephalopathy and Its Associated Neurodevelopmental Outcomes During the First Two Years of Life: A Retrospective Study in Saudi Arabia. Int J Gen Med. 2023;16:525-36.
Martinello K, Hart AR, Yap S, Mitra S, Robertson NJ. Management and investigation of neonatal encephalopathy: 2017 update. Arch Dis Child Fetal Neonatal Ed. 2017;102(4):F346-F58.
Tarvonen M, Hovi P, Sainio S, Vuorela P, Andersson S, Teramo K. Intrapartal cardiotocographic patterns and hypoxia-related perinatal outcomes in pregnancies complicated by gestational diabetes mellitus. Acta Diabetol. 2021;58(11):1563-73.
Jarmuzek P, Wielgos M, Bomba-Opon D. Placental pathologic changes in gestational diabetes mellitus. Neuro Endocrinol Lett. 2015;36(2):101-5.
Madazli R, Tuten A, Calay Z, Uzun H, Uludag S, Ocak V. The incidence of placental abnormalities, maternal and cord plasma malondialdehyde and vascular endothelial growth factor levels in women with gestational diabetes mellitus and nondiabetic controls. Gynecol Obstet Invest. 2008;65(4):227-32.
Radaelli T, Varastehpour A, Catalano P, Hauguel-de Mouzon S. Gestational diabetes induces placental genes for chronic stress and inflammatory pathways. Diabetes. 2003;52(12):2951-8.
Desoye G, Hauguel-de Mouzon S. The human placenta in gestational diabetes mellitus. The insulin and cytokine network. Diabetes Care. 2007;30 Suppl 2:S120-6.
Philips AF, Dubin JW, Matty PJ, Raye JR. Arterial hypoxemia and hyperinsulinemia in the chronically hyperglycemic fetal lamb. Pediatr Res. 1982;16(8):653-8.
Roberts KA, Riley SC, Reynolds RM, Barr S, Evans M, Statham A, et al. Placental structure and inflammation in pregnancies associated with obesity. Placenta. 2011;32(3):247-54.
Beneventi F, Locatelli E, Cavagnoli C, Simonetta M, Lovati E, Lucotti P, et al. Effects of uncomplicated vaginal delivery and epidural analgesia on fetal arterial acid-base parameters at birth in gestational diabetes. Diabetes Res Clin Pract. 2014;103(3):444-51.
Teramo KA, Widness JA. Increased fetal plasma and amniotic fluid erythropoietin concentrations: markers of intrauterine hypoxia. Neonatology. 2009;95(2):105-16.
Li HP, Chen X, Li MQ. Gestational diabetes induces chronic hypoxia stress and excessive inflammatory response in murine placenta. Int J Clin Exp Pathol. 2013;6(4):650-9.
Nancy Laval MP, Hamza Talsmat, Bohdana Marandyuk, Pia Wintermark, Ala Birca, Elana Pinchefsky, Sophie Tremblay. Exposure to maternal diabetes during pregnancy is associated with worse short-term neonatal and neurological outcomes following perinatal hypoxic-ischemic encephalopathy. PrePrint (Research Square). 2022.
Markiewicz I, Sypecka J, Domanska-Janik K, Wyszomirski T, Lukomska B. Cellular environment directs differentiation of human umbilical cord blood-derived neural stem cells in vitro. J Histochem Cytochem. 2011;59(3):289-301.
Chung DJ, Choi CB, Lee SH, Kang EH, Lee JH, Hwang SH, et al. Intraarterially delivered human umbilical cord blood-derived mesenchymal stem cells in canine cerebral ischemia. J Neurosci Res. 2009;87(16):3554-67.
Buzanska L, Machaj EK, Zablocka B, Pojda Z, Domanska-Janik K. Human cord blood-derived cells attain neuronal and glial features in vitro. J Cell Sci. 2002;115(Pt 10):2131-8.
Schira J, Falkenberg H, Hendricks M, Waldera-Lupa DM, Kogler G, Meyer HE, et al. Characterization of Regenerative Phenotype of Unrestricted Somatic Stem Cells (USSC) from Human Umbilical Cord Blood (hUCB) by Functional Secretome Analysis. Mol Cell Proteomics. 2015;14(10):2630-43.
Berlet R, Anthony S, Brooks B, Wang ZJ, Sadanandan N, Shear A, et al. Combination of Stem Cells and Rehabilitation Therapies for Ischemic Stroke. Biomolecules. 2021;11(9).
Zhao J, Chen N, Shen N, Zhao H, Wang D, Shi J, et al. Transplantation of human umbilical cord blood mesenchymal stem cells to treat a rat model of traumatic brain injury. Neural Regen Res. 2012;7(10):741-8.
CK L. An overview of cord blood stem cell transplantation in Hong Kong. Journal of Medical Science. 2022;91(3).
Shi PA, Luchsinger LL, Greally JM, Delaney CS. Umbilical cord blood: an undervalued and underutilized resource in allogeneic hematopoietic stem cell transplant and novel cell therapy applications. Curr Opin Hematol. 2022;29(6):317-26.
Serrenho I, Rosado M, Dinis A, C MC, Graos M, Manadas B, et al. Stem Cell Therapy for Neonatal Hypoxic-Ischemic Encephalopathy: A Systematic Review of Preclinical Studies. Int J Mol Sci. 2021;22(6).
Xi Y, Yue G, Gao S, Ju R, Wang Y. Human umbilical cord blood mononuclear cells transplantation for perinatal brain injury. Stem Cell Res Ther. 2022;13(1):458.
Archambault J, Moreira A, McDaniel D, Winter L, Sun L, Hornsby P. Therapeutic potential of mesenchymal stromal cells for hypoxic ischemic encephalopathy: A systematic review and meta-analysis of preclinical studies. PLoS One. 2017;12(12):e0189895.
Sun JM, Song AW, Case LE, Mikati MA, Gustafson KE, Simmons R, et al. Effect of Autologous Cord Blood Infusion on Motor Function and Brain Connectivity in Young Children with Cerebral Palsy: A Randomized, Placebo-Controlled Trial. Stem Cells Transl Med. 2017;6(12):2071-8.
Ullah M, Liu DD, Thakor AS. Mesenchymal Stromal Cell Homing: Mechanisms and Strategies for Improvement. iScience. 2019;15:421-38.
Zhou Y, Shao A, Xu W, Wu H, Deng Y. Advance of Stem Cell Treatment for Traumatic Brain Injury. Front Cell Neurosci. 2019;13:301.
Cotten CM, Murtha AP, Goldberg RN, Grotegut CA, Smith PB, Goldstein RF, et al. Feasibility of autologous cord blood cells for infants with hypoxic-ischemic encephalopathy. J Pediatr. 2014;164(5):973-9 e1.
Tsuji M, Sawada M, Watabe S, Sano H, Kanai M, Tanaka E, et al. Autologous cord blood cell therapy for neonatal hypoxic-ischaemic encephalopathy: a pilot study for feasibility and safety. Sci Rep. 2020;10(1):4603.
Malhotra A, Novak I, Miller SL, Jenkin G. Autologous transplantation of umbilical cord blood-derived cells in extreme preterm infants: protocol for a safety and feasibility study. BMJ Open. 2020;10(5):e036065.
Neuhoff S, Moers J, Rieks M, Grunwald T, Jensen A, Dermietzel R, et al. Proliferation, differentiation, and cytokine secretion of human umbilical cord blood-derived mononuclear cells in vitro. Exp Hematol. 2007;35(7):1119-31.
Watt SM, Gullo F, van der Garde M, Markeson D, Camicia R, Khoo CP, et al. The angiogenic properties of mesenchymal stem/stromal cells and their therapeutic potential. Br Med Bull. 2013;108(1):25-53.
Lee C, Shim S, Jang H, Myung H, Lee J, Bae CH, et al. Human umbilical cord blood-derived mesenchymal stromal cells and small intestinal submucosa hydrogel composite promotes combined radiation-wound healing of mice. Cytotherapy. 2017;19(9):1048-59.
Rai V, Moellmer R, Agrawal DK. Stem Cells and Angiogenesis: Implications and Limitations in Enhancing Chronic Diabetic Foot Ulcer Healing. Cells. 2022;11(15).
Yang G, Fan X, Liu Y, Jie P, Mazhar M, Liu Y, et al. Immunomodulatory Mechanisms and Therapeutic Potential of Mesenchymal Stem Cells. Stem Cell Rev Rep. 2023:1-18.
Huang Y, Wu Q, Tam PKH. Immunomodulatory Mechanisms of Mesenchymal Stem Cells and Their Potential Clinical Applications. Int J Mol Sci. 2022;23(17).
Galieva LR, Mukhamedshina YO, Arkhipova SS, Rizvanov AA. Human Umbilical Cord Blood Cell Transplantation in Neuroregenerative Strategies. Front Pharmacol. 2017;8:628.
Bojanic C, To K, Zhang B, Mak C, Khan WS. Human umbilical cord derived mesenchymal stem cells in peripheral nerve regeneration. World J Stem Cells. 2020;12(4):288-302.
Sung MA, Jung HJ, Lee JW, Lee JY, Pang KM, Yoo SB, et al. Human umbilical cord blood-derived mesenchymal stem cells promote regeneration of crush-injured rat sciatic nerves. Neural Regen Res. 2012;7(26):2018-27.
Andres RH, Horie N, Slikker W, Keren-Gill H, Zhan K, Sun G, et al. Human neural stem cells enhance structural plasticity and axonal transport in the ischaemic brain. Brain. 2011;134(Pt 6):1777-89.
Shi Y, Nan C, Yan Z, Liu L, Zhou J, Zhao Z, et al. Synaptic Plasticity of Human Umbilical Cord Mesenchymal Stem Cell Differentiating into Neuron-like Cells In Vitro Induced by Edaravone. Stem Cells Int. 2018;2018:5304279.